Abstract
Background: Patients with myelodysplastic syndrome with deletion of chromosome 5q (MDS del(5q)) have a favorable prognosis, but TP53 mutations occur in 13-18% of these patients and are known as unfavorable prognostic marker. Recently, Protein Phosphatase Magnesium-Dependent 1 (PPM1D) mutations have been described in clonal hematopoiesis and were found more commonly in patients with therapy-related MDS than in patients with primary MDS (15% vs. 3%) (Lindsley et al. 2017). PPM1D encodes a serine-threonine protein phosphatase that inhibits the p53 tumor suppressor pathway. It is therefore of great interest to evaluate the frequency and potential co-occurrence of PPM1D mutations in patients with MDS del(5q).
Aim: To determine the frequency and potential clinical impact of PPM1D mutations in a large cohort of MDS del(5q) patients.
Methods: 219 patients with MDS or AML following MDS (sAML) and deletion of chromosome 5q were included in the analysis. Patients were classified following the 2008 WHO classification. Patients with MDS (n=196) or sAML (n=23) were cytogenetically characterized by chromosome banding analysis and molecularly analyzed for mutations in all exons (1 to 6) of PPM1D by Sanger or next-generation sequencing (NGS). Patients were also analyzed for mutations in TP53 and CSNK1A1 .
Results: A total of 11 PPM1D mutations were found in 10 (4.6%) MDS patients with del(5q). The mutation frequency was similar in patients with MDS with isolated del5q (8 of 167, 4.8%) compared to patients with more advanced MDS or secondary AML (2 of 52, 3.8%, P=.78). Four patients had nonsense mutations, 3 patients had frameshift mutations (one patient with 2 frameshift mutations), and 3 patients had missense mutations. Nine mutations were found in the previously described hotspot region of PPM1D between amino acids 427 and 542, which is located downstream of the phosphatase domain of PPM1D. Three of the 10 PPM1D mutated patients had additional cytogenetic aberrations besides del(5q) (trisomy 8; complex karyotype in two patients). TP53 was also mutated in the two patients with complex karyotype and in one additional patient with a nonsense mutation of PPM1D . None of the PPM1D mutated patients had a mutation in CSNK1A1 .
Patients with mutated PPM1D were slightly older than PPM1D wildtype patients (median age 77.7 vs 71 years, not significant). Eight of 10 PPM1D mutated patients had a diagnosis of MDS del(5q) and 2 patients had MDS RAEB2 with del(5q) accompanied by a complex karyotype. There were no significant differences in the distribution of sex, WHO subtypes, cytogenetic risk according to the international prognostic scoring system (IPSS), WBC count, hemoglobin, platelet count and IPSS risk score between PPM1D wildtype and mutated patients. Two of the 10 patients were transfusion dependent and none of 7 patients with available information transformed to AML.
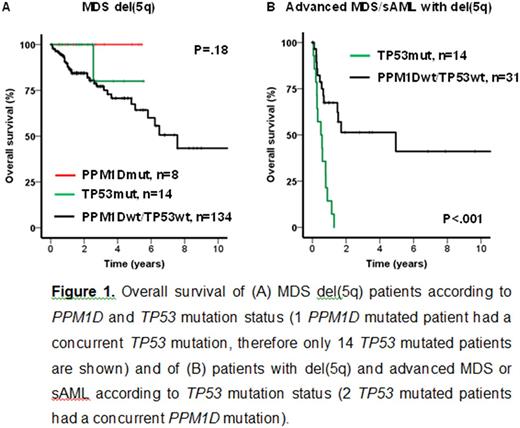
Survival information was available for 156 patients with MDS del(5q) (excluding other WHO subtypes of MDS/sAML) including 8 patients with mutated PPM1D and 15 patients with mutated TP53 . Median follow-up from the time of sample harvest was 2.5 years. The probability of survival at 2 years was 100% for PPM1D mutated and TP53 mutated patients, respectively, and 84% for PPM1D/TP53 wildtype patients (P=.18, log-rank test, Figure 1A). None of 7 PPM1D mutated patients and 1 of 13 TP53 mutated patients with available information underwent allogeneic hematopoietic cell transplantation.
Survival information was available for 45 patients with del(5q) and more advanced MDS or secondary AML. The 14 patients with TP53 mutation (including 2 patients with additional PPM1D mutation) had a significantly shorter OS than TP53 wildtype patients (P<.001, 2-year OS 0% vs 51%, Figure 1B). One PPM1D mutated patient responded well to lenalidomide treatment for the duration of 3.2 years.
Conclusion: PPM1D mutations are recurrently mutated in MDS patients with del(5q) with a frequency of 4.6% and may co-occur with TP53 mutations. PPM1D mutated patients were not specifically associated with patient characteristics or outcome. Interestingly, in our cohort of patients with MDS with isolated del(5q), TP53 mutations were not associated with unfavorable outcome.
VP and MM contributed equally as first authors. TH and MH contributed equally as last authors.
Meggendorfer: MLL Munich Leukemia Laboratory: Employment. Haferlach: MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Platzbecker: Novartis: Consultancy, Research Funding; Acceleron: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding. Thiede: Novartis: Consultancy, Speakers Bureau; Roche: Consultancy; Agendix: Employment; Bayer: Consultancy, Speakers Bureau. Germing: Novartis: Honoraria, Research Funding; Janssen: Honoraria; Celgene: Honoraria, Research Funding. Schroeder: Celgene: Consultancy, Honoraria, Other: travel support. Kobbe: Celgene: Other: Advisory Board, Research Funding. Haase: Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Consultancy, Honoraria, Research Funding. Dohner: Novartis: Honoraria, Research Funding. Sperr: Novartis: Other: Register; Phadia: Research Funding; Meda: Research Funding; Celgene: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding; Teva: Honoraria. Valent: Novartis: Honoraria, Research Funding; Ariad: Honoraria, Research Funding; Incyte: Honoraria; Blueprint: Research Funding; BMS: Honoraria; Celgene: Honoraria, Research Funding; Pfizer: Honoraria; Deciphera: Honoraria, Research Funding; Teva: Honoraria. Haferlach: MLL Munich Leukemia Laboratory: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.